Comprehensive Guide to Self-Monitoring of Glucose Levels: Tips To Ensure You Accurately Get Your Sugar Levels Right.
JANE Blog blood glucose, blood sugar, blood sugar levels, blood sugar testing, CGM, diabetes care, Diabetes Management, diabetes tips, glucometer, glucose levels, Health monitoring, hyperglycemia, hypoglycemia, self-monitoring 0
Managing diabetes effectively requires constant vigilance and understanding of your blood sugar levels. Self-monitoring of blood glucose (SMBG) is a cornerstone in diabetes management, enabling individuals to track their glucose levels at home and make informed decisions about their health. This comprehensive guide will explore the various aspects of SMBG, from the basics to advanced monitoring techniques, providing you with the knowledge needed to maintain optimal health.
What Are Blood Sugar Levels?
Blood sugar, or glucose, is the primary sugar found in your blood and serves as your body’s main source of energy. Glucose levels fluctuate throughout the day, influenced by factors like food intake, physical activity, and stress. Understanding these fluctuations and maintaining target blood sugar levels is crucial, especially for individuals with diabetes.
Normal Blood Sugar Levels
For most people without diabetes, normal fasting blood sugar levels range from 70 to 99 mg/dL. Two hours after eating, levels should be less than 140 mg/dL. These ranges are essential for maintaining overall health and preventing complications.
Abnormal Blood Sugar Levels
- Hypoglycemia (Low Blood Sugar): Blood sugar levels below 70 mg/dL. Symptoms include shakiness, sweating, confusion, and dizziness.
- Hyperglycemia (High Blood Sugar): Blood sugar levels above 180 mg/dL two hours after eating. Symptoms include frequent urination, increased thirst, and fatigue.
Maintaining these levels within the normal range helps prevent both short-term and long-term complications, such as diabetic ketoacidosis and cardiovascular diseases.
Why Monitor Blood Sugar Levels?
Monitoring blood sugar levels provides critical insights into how your body responds to various factors and helps in managing diabetes effectively. Here are some key reasons for regular monitoring:
- Effective Diabetes Management: Regular monitoring helps in making informed decisions about diet, exercise, and medication adjustments.
- Understanding Body Responses: It helps in understanding how your body reacts to different foods, physical activities, and stress.
- Recognizing Triggers: Identifying triggers for blood sugar spikes or crashes can help in avoiding them.
- Evaluating Treatment Goals: Monitoring allows you and your healthcare provider to assess the effectiveness of your current treatment plan and make necessary adjustments.
Benefits of Regular Monitoring
- Prevention of Complications: Regular monitoring helps in early detection of blood sugar abnormalities, preventing complications.
- Personalized Treatment Adjustments: Based on your readings, your healthcare provider can tailor your treatment plan to better suit your needs.
- Improved Quality of Life: Better blood sugar control leads to fewer symptoms and a higher quality of life.
How to Monitor Blood Sugar Levels at Home
There are several methods for monitoring blood glucose levels at home, primarily using glucometers and continuous glucose monitors (CGMs).
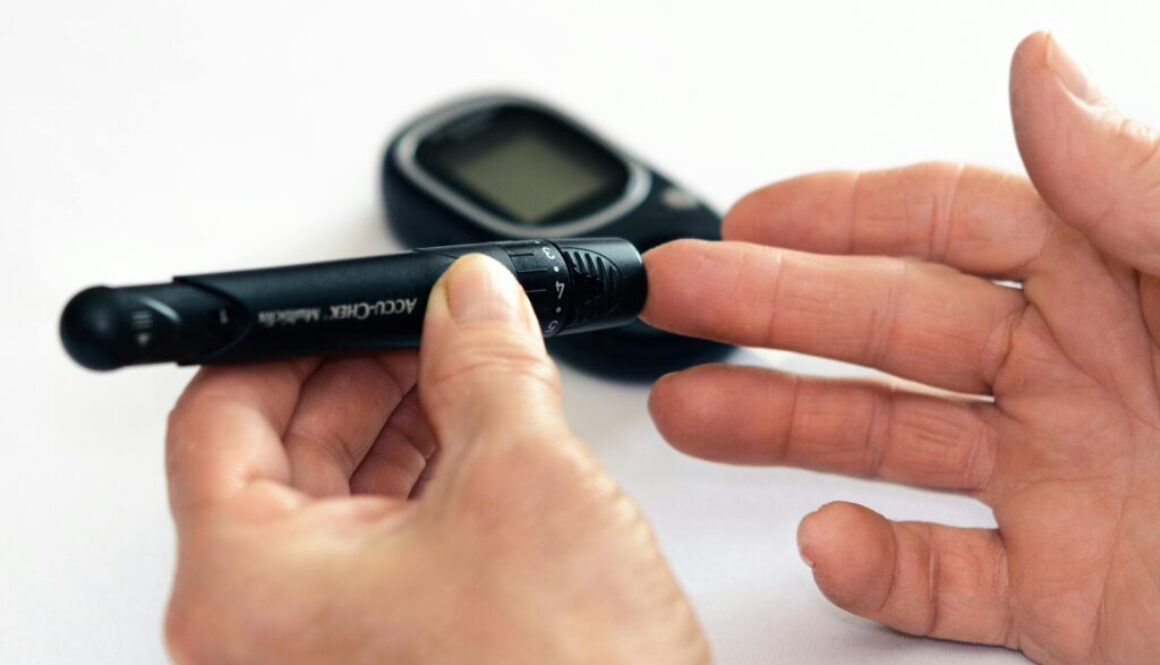
Using a Glucometer
A glucometer is a small, portable device that provides instant feedback on your blood sugar levels. Here’s a detailed guide on how to use it:
- Insert a Test Strip: Start by inserting a test strip into the device.
- Prick Your Finger: Use a lancet device to prick your finger and obtain a drop of blood.
- Apply Blood to the Strip: Place the drop of blood on the test strip.
- Read the Result: Wait for the glucometer to display your blood sugar level.
Features and Benefits of Glucometers
- Instant Feedback: Glucometers provide quick results, allowing immediate action if your blood sugar levels are abnormal.
- Portability: These devices are small and easy to carry, making them convenient for regular use.
- Versatility: They help manage various types of diabetes by showing if blood sugar levels are too high, too low, or within the target range.
Continuous Glucose Monitors (CGMs)
CGMs offer a more comprehensive way to track blood glucose levels. These devices continuously monitor glucose levels throughout the day and night, providing real-time data and alerts for high or low blood sugar levels. CGMs consist of a small sensor placed under the skin that measures glucose levels in interstitial fluid. The data is transmitted to a display device or smartphone app.
Advantages of CGMs
- Real-Time Monitoring: Continuous updates on glucose levels help in proactive diabetes management.
- Alerts: CGMs can alert you to dangerous blood sugar levels, allowing for immediate corrective action.
- Comprehensive Data: They provide detailed trends and patterns, helping to understand blood sugar fluctuations over time.
How to Perform a Finger-Prick Test
A finger-prick test is a common method for checking blood sugar levels using a glucometer. Here’s a step-by-step guide:
- Wash Your Hands: Clean hands ensure accurate readings.
- Prepare the Lancet Device: Insert a new lancet into the device.
- Insert a Test Strip: Place a test strip into the glucometer.
- Prick Your Finger: Use the lancet device to prick the side of your fingertip.
- Squeeze Out a Drop of Blood: Gently squeeze your finger to get a drop of blood.
- Apply the Blood: Place the blood on the test strip.
- Read the Result: Wait for the glucometer to display your blood sugar level.
Tips for Minimizing Pain
- Rotate Fingers: Avoid using the same finger repeatedly to reduce soreness.
- Use Fresh Lancets: Always use a new, sharp lancet to minimize discomfort.
- Prick the Side of the Finger: The sides of the fingertips are less painful than the pads.
Interpreting Blood Sugar Readings
Understanding your blood sugar readings is essential for effective diabetes management. Here’s how to interpret the results:
What’s My Target Range?
Your target range may vary based on your overall health and treatment plan. General target ranges include:
- Fasting Blood Sugar: 70-99 mg/dL for non-diabetics. Your doctor may set a different range if you have diabetes.
- Postprandial (After Meal) Blood Sugar: Less than 140 mg/dL two hours after eating for non-diabetics.
Low Blood Sugar (Hypoglycemia)
- Symptoms: Shakiness, sweating, confusion, dizziness, hunger, irritability.
- Immediate Actions: Consume fast-acting carbohydrates such as glucose tablets, fruit juice, or regular soda.
High Blood Sugar (Hyperglycemia)
- Symptoms: Frequent urination, increased thirst, blurred vision, fatigue, headache.
- Immediate Actions: Follow your healthcare provider’s instructions, which may include taking medication, drinking water, or adjusting your diet and exercise.
Tracking Blood Sugar Levels
Keeping a log of your blood sugar readings helps in identifying patterns and trends. It also provides valuable information for your healthcare provider.
Methods to Record Your Readings
- Paper Logs: Simple and easy to use.
- Digital Apps: Convenient and often integrate with your glucometer or CGM.
- Integrated Systems: Some glucometers and CGMs come with integrated tracking systems that automatically record your readings.
Blood Sugar Monitoring Throughout the Day
When and how often to check your blood sugar depends on your specific situation and type of diabetes.
When to Check Blood Sugar Levels
- Before Meals: Helps determine insulin needs and provides a baseline reading.
- After Meals: Provides insight into how your body handles food.
- Before and After Exercise: Ensures safe blood sugar levels during physical activity.
- At Bedtime: Helps prevent nocturnal hypoglycemia.
- During Stress or Illness: Blood sugar can fluctuate significantly during these times.
How Often Should You Check Your Blood Sugar?
The frequency of testing varies based on individual needs and type of diabetes:
- Type 1 Diabetes: Often requires multiple checks per day.
- Type 2 Diabetes: Frequency varies depending on whether you’re managing your diabetes with insulin, oral medications, or diet and exercise alone. Your healthcare provider will guide you.
Risks and Benefits of SMBG
Benefits
- Better Diabetes Management: Allows for more precise adjustments to diet, exercise, and medication.
- Prevention of Complications: Helps in avoiding both short-term and long-term complications by detecting abnormal blood sugar levels early.
- Personalized Treatment Adjustments: Data-driven decisions lead to better health outcomes.
- Improved Quality of Life: Better blood sugar control leads to fewer symptoms and a higher quality of life.
Risks
- Fingertip Pain: Frequent testing can cause discomfort.
- Cost: Test strips, lancets, and CGMs can be expensive.
- Negative Emotions: Stress and anxiety from frequent testing and monitoring.
Common Issues and Troubleshooting
Preventing Sore Fingertips
- Rotate Testing Sites: Use different fingers and alternate sites on the fingers.
- Proper Technique: Prick the side of your fingertip rather than the pad.
Ensuring Accurate Readings
- Store Test Strips Properly: Keep them in a cool, dry place and check the expiration date.
- Calibrate Devices: Regular calibration of your glucometer ensures accuracy. Follow the manufacturer’s instructions.
- Clean Hands: Always wash your hands before testing to avoid contamination.
Things to Watch Out For
- Symptoms of Abnormal Glucose Levels: Recognize and respond promptly to signs of hypoglycemia and hyperglycemia.
- Device Malfunctions: Ensure your glucometer or CGM is functioning correctly. Replace batteries regularly and check for any error messages.
When to Contact Your Healthcare Provider
Regular communication with your healthcare provider is crucial for effective diabetes management.
Situations Requiring Medical Attention
- Persistent High or Low Blood Sugar Levels: Continuous abnormal readings need medical evaluation.
- Unexplained Fluctuations: Sudden changes without a clear cause should be discussed with your healthcare provider.
- Signs of Infection: Especially at the finger-prick sites. Look for redness, swelling, or pus.
Emergency Situations
- Severe Hypoglycemia: If you experience severe symptoms such as unconsciousness, seek emergency care immediately.
- Diabetic Ketoacidosis: Symptoms include high blood sugar, ketones in urine, nausea, and vomiting. This requires urgent medical attention.
Frequently Asked Questions
Can I Check My Own Blood Sugar?
Yes, with a glucometer or CGM, you can check your own blood sugar levels at home. These devices are designed for ease of use and provide quick results.
How Often Should I Check My Blood Sugar?
This depends on your treatment plan and type of diabetes. People with Type 1 diabetes may need to check multiple times a day, while those with Type 2 diabetes might check less frequently. Your healthcare provider will give you specific recommendations.
What Should I Ask My Provider About Blood Sugar Monitoring?
- What is my target blood sugar range?
- How often should I check my blood sugar?
- What should I do if my blood sugar is too high or too low?
- How can I adjust my diet, exercise, and medication based on my readings?
Conclusion
Self-monitoring of blood glucose is an essential practice for individuals with diabetes. It provides valuable insights into your body’s response to various factors and helps in managing the condition effectively. By using tools like glucometers and CGMs, following a structured monitoring routine, and maintaining regular communication with your healthcare provider, you can take control of your health and lead a fulfilling life.
This comprehensive guide aims to provide valuable information for anyone looking to understand and implement self-monitoring of glucose levels. By following these practices, you can effectively manage your diabetes and lead a healthier life.