Insulin: The Hormone Regulating Blood Sugar And Everything You Need To Know to Ensure You Are Healthy
Introduction
Blood sugar regulation is crucial for maintaining overall health. Insulin and glucagon are the primary hormones responsible for this process. Understanding how these hormones work can help manage conditions like diabetes. This guide provides an in-depth look at how insulin and glucagon maintain normal blood sugar levels.
Fuels of the Body
Glucose: The Primary Fuel
Glucose is the main energy source for the body. It is essential for brain function, muscle activity, and overall metabolism. When you eat carbohydrates, your body breaks them down into glucose, which enters your bloodstream. From there, glucose is transported to cells to be used as energy.
Alternative Fuels: Ketones and Glycogen
When glucose levels are low, the body uses alternative fuels such as ketones and glycogen. Ketones are produced from fat and serve as an important energy source during fasting or low-carbohydrate diets. Glycogen, on the other hand, is stored glucose in the liver and muscles. During periods of low blood sugar, glycogen is broken down into glucose to provide a quick source of energy.
Hormones of the Pancreas
Insulin
Insulin is produced by beta cells in the pancreas. It plays a crucial role in lowering blood sugar levels by facilitating the uptake of glucose into cells and converting it into glycogen. This hormone is essential for maintaining energy balance and preventing hyperglycemia (high blood sugar). When blood sugar levels rise after eating, the pancreas releases insulin to help cells absorb glucose from the bloodstream.
Glucagon
Glucagon is produced by alpha cells in the pancreas. It raises blood sugar levels by converting stored glycogen back into glucose, which is then released into the bloodstream. This process, known as glycogenolysis, ensures that your body has a steady supply of glucose during periods of fasting or between meals. Glucagon is crucial for preventing hypoglycemia (low blood sugar).
Amylin
Amylin is released along with insulin from the beta cells of the pancreas. It helps regulate blood sugar by slowing gastric emptying and decreasing glucagon levels. Amylin also promotes satiety, which can help prevent overeating and subsequent spikes in blood sugar levels.
Incretins (GLP-1 and GIP)
GLP-1 (Glucagon-Like Peptide-1) and GIP (Gastric Inhibitory Polypeptide) are hormones that enhance insulin secretion and reduce glucagon release. They are part of a group of hormones known as incretins. In addition to their effects on insulin and glucagon, incretins also slow food emptying from the stomach and promote feelings of fullness, which helps regulate post-meal blood sugar levels.
How Insulin Works
Mechanism of Action
Insulin helps cells absorb glucose from the bloodstream, thereby lowering blood sugar levels. It also signals the liver to store glucose as glycogen. This process is crucial for maintaining energy balance in the body. When insulin binds to its receptors on the surface of cells, it triggers a series of reactions that allow glucose to enter the cells and be used for energy or stored for later use.
Types of Insulin for Diabetes
There are several types of insulin used to manage diabetes, each with different onset times, peak effects, and durations:
- Rapid-Acting Insulin: Begins to work within 15 minutes and peaks at about 1-2 hours. Examples include insulin lispro (Humalog) and insulin aspart (NovoLog).
- Short-Acting Insulin: Starts working within 30 minutes and peaks at 2-3 hours. Examples include regular insulin (Humulin R, Novolin R).
- Intermediate-Acting Insulin: Begins to work in 2-4 hours, peaks at 4-12 hours. Examples include NPH insulin (Humulin N, Novolin N).
- Long-Acting Insulin: Takes several hours to start working and lasts up to 24 hours. Examples include insulin glargine (Lantus) and insulin detemir (Levemir).
Basal vs. Bolus Insulin
Basal insulin provides a steady level of insulin throughout the day and night, mimicking the body’s natural insulin production. It helps maintain blood sugar levels in the fasting state. Bolus insulin, on the other hand, is taken at meal times to manage blood sugar spikes that occur after eating. This approach, known as basal-bolus therapy, provides comprehensive blood sugar control for individuals with diabetes.
Starting Insulin Therapy
Starting insulin therapy involves determining the right type and dose for the individual. This process is tailored based on blood sugar levels, lifestyle, and the type of diabetes. It often begins with a low dose of long-acting insulin, which may be adjusted over time. For some, a combination of basal and bolus insulin may be necessary to achieve optimal blood sugar control.
How to Inject Insulin for Diabetes
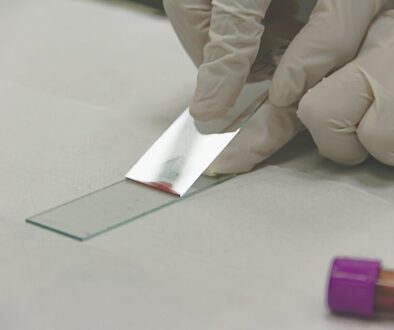
Proper insulin injection techniques are crucial for effective management. Here is a step-by-step guide:
- Wash Your Hands: Ensures cleanliness and reduces the risk of infection.
- Prepare the Injection: Check the insulin for any abnormalities and ensure it is at the right temperature.
- Choose an Injection Site: Common sites include the abdomen, thigh, and upper arm. Rotate sites to avoid tissue damage.
- Clean the Injection Site: Use an alcohol swab to clean the area.
- Inject the Insulin: Pinch the skin, insert the needle at a 90-degree angle (or 45-degree if using a longer needle), and press the plunger.
- Dispose of Needles Safely: Use a sharps container to dispose of needles.
Traveling with Insulin
Managing insulin while traveling requires careful planning. Here are some tips:
- Keep Insulin Cool: Use insulated bags or travel coolers to keep insulin at the right temperature.
- Carry Supplies: Bring enough insulin, needles, and other supplies for the entire trip, plus extras.
- Time Zone Adjustments: Adjust your insulin schedule based on the time zone changes.
- Prescription and Documentation: Carry a prescription and a letter from your doctor explaining your need for insulin.
The Role of Glucagon
Function of Glucagon
Glucagon raises blood sugar levels by breaking down glycogen stores in the liver. This process, known as glycogenolysis, releases glucose into the bloodstream, ensuring a steady supply of energy. Glucagon is particularly important during fasting or between meals when blood sugar levels drop.
Glucagon vs. Insulin
Insulin and glucagon have opposite effects but work together to maintain blood sugar balance. While insulin lowers blood sugar by facilitating glucose uptake into cells, glucagon raises blood sugar by promoting glycogen breakdown in the liver. This interplay ensures that blood sugar levels remain within a narrow, healthy range.
Glucagon vs. Glycogen
It is important to distinguish between glucagon and glycogen. Glucagon is a hormone that triggers the conversion of glycogen to glucose. Glycogen is the stored form of glucose in the liver and muscles. Glucagon signals the liver to break down glycogen into glucose, which is then released into the bloodstream.
Tests and Levels
Glucagon levels can be measured through blood tests. Normal glucagon levels vary, but significant deviations can indicate health issues. High glucagon levels can suggest conditions like glucagonoma, while low levels might indicate issues with pancreatic function.
Conditions Related to Glucagon Function
Abnormal glucagon levels can lead to conditions such as:
- Glucagonoma: A rare tumor of the pancreas that secretes excessive glucagon, leading to hyperglycemia.
- Hypoglycemia: Low blood sugar levels due to insufficient glucagon or impaired glycogen breakdown.
Symptoms of these conditions can include weight loss, skin rash, and high or low blood sugar levels. Proper diagnosis and treatment are crucial for managing these conditions effectively.
The Role of Other Hormones
Amylin
Amylin complements insulin’s action by regulating blood sugar levels. It slows gastric emptying, suppresses glucagon secretion, and promotes satiety. These effects help prevent post-meal blood sugar spikes and improve overall blood sugar control.
Epinephrine
Epinephrine, also known as adrenaline, promotes the production of glucose in the liver and the breakdown of fat for energy. It helps the body respond to stress by increasing blood sugar levels, providing a quick source of energy during the fight-or-flight response.
Poor Regulation of Blood Glucose
Insulin Resistance
Insulin resistance occurs when cells do not respond effectively to insulin. This leads to higher blood sugar levels and can result in type 2 diabetes. Factors contributing to insulin resistance include obesity, physical inactivity, and genetics. Managing insulin resistance involves lifestyle changes such as a healthy diet, regular exercise, and weight loss.
Beta Cell Dysfunction
Beta cell dysfunction impairs insulin production. This can contribute to the development of diabetes, as the body cannot regulate blood sugar effectively. Causes of beta cell dysfunction include genetic factors, chronic inflammation, and exposure to certain toxins. Treatment typically involves medications that improve beta cell function or supplement insulin production.
Cell Damage in Diabetes Mellitus (DM)
Chronic high blood sugar damages cells and tissues, leading to complications such as:
- Neuropathy: Nerve damage that causes pain, tingling, or loss of sensation.
- Retinopathy: Damage to the blood vessels in the eyes, leading to vision problems.
- Nephropathy: Kidney damage that can progress to kidney failure.
- Cardiovascular Disease: Increased risk of heart disease and stroke.
Managing blood sugar levels effectively is crucial for preventing these complications.
Health Conditions Related to Blood Sugar Regulation
Glucose Disorders
Disorders like hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) require careful management to prevent complications. Hypoglycemia can cause symptoms like shakiness, sweating, and confusion, while hyperglycemia can lead to increased thirst, frequent urination, and fatigue.
Symptoms and Diagnosis
Symptoms of glucose disorders include:
- Hypoglycemia: Shakiness, sweating, confusion, rapid heartbeat.
- Hyperglycemia: Increased thirst, frequent urination, fatigue, blurred vision.
Diagnostic tests measure blood sugar levels and hormone function. Common tests include fasting blood sugar, oral glucose tolerance test, and hemoglobin A1c.
When to Talk to a Doctor
Seek medical advice if you experience symptoms of abnormal blood sugar levels. Early diagnosis and treatment are crucial for effective management. Regular check-ups and monitoring can help prevent complications and improve quality of life.
Practical Tips and Takeaways
Maintaining Ideal Blood Sugar Levels
Maintain blood sugar within the target range through a balanced diet, regular exercise, and medication adherence. Monitoring blood sugar levels regularly can help you make informed decisions about your health.
Lifestyle and Dietary Considerations
A healthy diet rich in fiber, lean protein, and healthy fats helps manage blood sugar. Foods that have a low glycemic index (GI) are particularly beneficial as they cause a slower, more gradual rise in blood sugar. Regular physical activity also improves insulin sensitivity and helps maintain a healthy weight.
Dietary Tips:
- High-Fiber Foods: Vegetables, fruits, whole grains, legumes.
- Lean Proteins: Chicken, fish, tofu, legumes.
- Healthy Fats: Avocados, nuts, seeds, olive oil.
Monitoring and Management
Use tools like glucose meters and continuous glucose monitors to track blood sugar levels. Regular monitoring helps adjust treatment plans as needed. Keeping a log of your readings can help identify patterns and triggers that affect your blood sugar.
Management Tools:
- Glucose Meters: Portable devices that measure blood sugar levels from a drop of blood.
- Continuous Glucose Monitors (CGMs): Devices that measure blood sugar levels continuously throughout the day and night.
- Insulin Pumps: Devices that deliver a continuous supply of insulin through a small tube inserted under the skin.
Conclusion
Understanding insulin and glucagon’s roles in blood sugar regulation is essential for managing diabetes and maintaining health. By leveraging knowledge and practical strategies, you can effectively manage blood sugar levels and prevent complications.
FAQs
Q: How often should I check my blood sugar levels? A: It depends on your treatment plan. Typically, people with diabetes should check their blood sugar multiple times a day.
Q: What foods can help stabilize blood sugar levels? A: Foods high in fiber, lean proteins, and healthy fats can help stabilize blood sugar levels.
Q: Can stress affect blood sugar levels? A: Yes, stress can cause blood sugar levels to rise due to the release of stress hormones like cortisol and epinephrine.
Q: What is the best time to inject insulin? A: This varies depending on the type of insulin. Basal insulin is usually taken once daily, while bolus insulin is taken before meals.
Q: How can I manage my blood sugar levels while traveling? A: Plan ahead by carrying enough supplies, keeping insulin at the right temperature, and maintaining your usual eating and exercise routines.